Under the Microscope: #3 Organs Examination
The thoracic and abdominal viscera are laid on a cutting bench at a convenient height and under good illumination. Ample washing water should be available from a flexible pipe, to flush the tissues as dissection proceeds. Some pathologists maintain that this should not be done, as the water can have an effect on the quality of subsequent histological sections, but this has recently been disproved. In any case, the vastly inferior naked-eye examination that results if blood is not removed at frequent intervals greatly outweighs any unsubstantiated objections about the more exquisite details of cell structure, especially as in most forensic autopsies the gross appearances are usually far more important. The viscera should be laid so that the tongue faces the pathologist, with the aorta upwards. The same sequence of examination should be carried out whatever the nature of the case, so that a fixed routine will ensure that nothing is left undone.
The tongue is examined for disease and injuries, including bites suggesting blows in the jaw or epilepsy. The tongue should be sliced to detect deep hemorrhages sometimes seen in strangulation. Such hemorrhage is seen mostly at the sides and center of the mid-part of the tongue. Gross congestion, which may be due to either pressure on the neck or to other congestive modes of death, is usually in the posterior part of the tongue. The tonsils and pharyngeal walls are inspected. The glottis is examined for mechanical or infective obstruction, and the hyoid and thyroid horns palpated for fractures. The oesophagus is opened with large (20 cm) bluntnosed scissors, which along with a very sharp 10-15cm bladed knife and a long-bladed 'brain knife', are the most useful tools for performing an autopsy.
The carotid arteries on each side are opened, including. The bifurcation and sinuses. If necessary, the upper portions of the carotids are explored in the body itself and followed to the base of the skull. If thrombosis is suspected, the intracranial part should be examined in the cavernous sinus. Returning to the neck structures, the thyroid should be sliced and inspected, then the oesophagus opened almost to the cardia of the stomach and any suspect material such as . . capsules, tablets or powder retained for analysis. The scissors are then passed down the posterior line of the larynx and trachea to the carina. If pressure on the neck of any type, such as strangulation, is suspected, then special examination should be made. The trachea and main bronchi should be inspected for disease and obstruction. The trachea and main bronchi should be inspected for disease and obstruction. Gastric contents are often found.
The overall process to thoroughly
examine the body goes to lungs. The lungs are removed, after careful
examination of their external surfaces for patchy collapse, emphysema, petechiae
and so on. Almost every autopsy will reveal a few petechiae, especially around
the hilum and in the interlobar fissures. The lungs are removed from the thoracic pluck
by passing a long-bladed knife (such as a brain knife) under the hilum with the
blunt edge upwards. The knife is settled in the correct posirion hefnre turning
the sharp edge upwards to cut through the hilum. Before doing this it may be
necessary to remove adhesions over the diaphragm and to cut through the pulmonary
ligament, a thin sheet of tissue that ties the inferior medial edge of the
lower lobe to the mediastinum. As the hilum is being cut, the pathologist must
notice if any embolism is visible within the pulmonary arteries. It has happened
that such an embolism has slid out and been washed unnoticed down the sink.
Some pathologists insist on opening the main pulmonary trunk and even right
ventricle before removing the lungs, to seek a saddle embolus. This is not
necessary, as any large embolus will be readily visible on examining the heart
and the lungs in the usual sequence.
Both lungs are taken off and the hilurn inspected before being laid aside for cutting. The lung should be weighed before cutting, as appreciable oedema fluid can run away during dissection. Then each is laid with the hilum down on the dissecting board, the opportunity being taken during handling to evaluate weight and oedema, as well as emphysema. The lung is held on the upper surface by the left hand of the operator (or by an interposed sponge) and the organ cut across in the sagittal plane from apex to base with the large brain knife, held parallel to the board. This produces an anteroposterior slice, the lower medial part carrying the hilum. The cut surfaces can now be opened like a book and the surface examined for oedema, tumour, pneumonias, infarction, trauma and so on. The smaller bronchi must be inspected for such signs as mucosal thickening, infection and blockage. The smaller pulmonary arteries may reveal thrombosis or embolism that was not visible in the larger vessels.
In some medico-legal autopsies, especially in industrial lung disease such as pneumoconiosis or asbestosis, one or both lungs need to be inflated with formalin for fixation before cutting. This preserves the shape and histology in excellent condition, but delays examination for at least several days. It is carried out by holding or tying a cannula into the bronchus while 10 per cent form01 saline is perfused through a tube from a reservoir held about 1 metre above the lung. The lung is then left in a bath of formalin covered with a formalin-soaked cloth to prevent drying.
There are almost as many ways of
examining the heart as there are pathologists, and each operator must decide
upon the method that appeals most. In this summary there is no space for
discussion of post-mortem angiography, which is moving from the field of
research and special interest into routine use. A common and practical routine
for examining the heart is described here. First, the organ mass minus the
lungs is rotated so that the lower end now faces the pathologist. The scissors
are passed into the cut end of a common iliac artery and passed right up to the
aortic arch and around to a few centimetres above the aortic valve, staying
outside the reflection of the pericardium. The interior of the aorta is
studied, especially for the degree of atheroma and for any aneurysms or trauma.
The inferior vena cava is opened from its lower end into the liver. The organ
pluck is then turned over so that the heart is uppermost. The pericardiurn is
inspected externally for fluid and blood tamponade, then opened widely with
scissors. The heart is delivered through the incision and inspected externally
for pericarditis, adhesions, discoloration of an underlying infarct and cardiac
aneurysms, for example. In a child, the thymus would be inspected and dissected
off at this stage.
The heart is then removed by
holding it up with the left hand so that its attachment is tensed against the
other organs. A long knife, such as a brain knife, is then passed horizontally
across at the reflection of the pericardium, cutting through the root of the
aorta and other great vessels just above the atria. The now-detached heart is
washed externally and placed in the anatomical position on the dissecting
board, with the apex facing the operator and the anterior surface upwards. It
should not be weighed until all the contained blood and clot is removed. The
general size, shape and ventricular preponderance should be noted. Any
dilatation or thickening of the pulmonary conus should be noted as an index of right
ventricular hypertrophy, especially if striae of transverse muscle fibres are
seen crossing the conus.
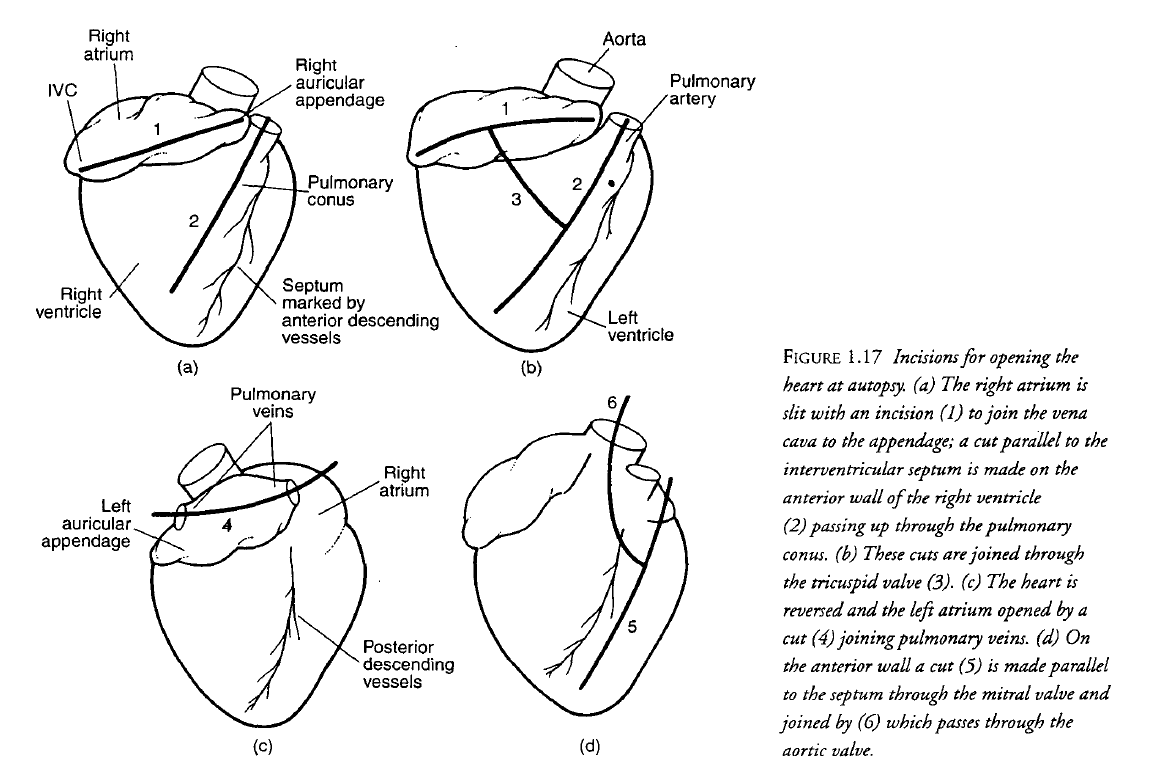
The right atrium is then opened by introducing scissors into the inferior vena cava and cutting- across to the atrial appendage. The interior of the atrium is examined and the septum and tricuspid valve inspected. The interventricular septum is then identified externally by the vessels running down the outside. With a knife a cut is made about 15 mm to the right of and parallel to the septum, over the right ventricle. This should be deep enough to enter the lumen, but not enough to cut the posterior wall. The scissors are now introduced into the cut and run up through the pulmonary conus and into the pulmonary artery until they meet the transected end. They are also extended downwards to the apex of the ventricle. The scissors are now put in midway down this linear cut and passed outwards at right angles, guided by the fingers of the left hand passed into the tricuspid valve from the opened atrium. The whole of the right side of heart is now open and displayed. It should be washed out and the endocardium and valve examined. A similar routine is now employed on the left side. The scissors are introduced into a pulmonary vein and passed horizonrally across to an opposite vein, thus opening the atrium. Fingers are introduced down through the mitral valve to estimate its size and detect any stenosis.
After weighing, the endocardium and valves are examined, then the coronary arteries. Once again, controversy exists about methods of opening the coronary vessels, but the weight of opinion now lies almost universally with those who cut serial interrupted cross-sections with a knife, rather than open them longitudinally with small scissors.
Cutting across the vessels allows an estimate of the percentage stenosis. It is admitted that this may not be the size of the lumen during life when normal blood pressure is operating, but the same disadvantage applies to longitudinal opening. An estimate of luminal size is relatively constant, however, in that the collapsed abnormal can still be compared with the collapsed normal. The coronaries are therefore cut across at frequent intervals. Before the first cut, the ostia are examined for congenital variations (which are frequent) and for obstruction. The left coronary artery is then cut across from the epicardial surface, starting as close to the ostium as possible, as occlusion and severe stenosis can occur very near the origin. Serial cuts are then made at intervals of not more than 3 mm, first into the common trunk, then following the lefi circumflex laterally until the vessel becomes too small, usually when it dips down from the epicardium to become intramuscular. The anterior descending branch is then followed down the front of the septum almost to the apex. Turning to the right coronary artery, the proximal segment is cut back from the point where the right ventricle was opened, transecting the artery in its mid-part. The cuts are made back to the aorta, then the distal segment is followed laterally until it becomes the posterior descending branch. During this process, the dominance of right versus left vessels is noted. Difficulty arises where severe calcification exists, as the knife either fails to cut through the artery or shatters it because of the excessive force required. The lumen is crushed and the percentage stenosis is difficult or impossible to assess. Scissors may be used to exert more force than a knife, but the only real solution is to decalcify the vessels.
Except for research purposes, it
must be admitted that the days or even weeks of delay occasioned by
decalcification provide a formidable deterrent for the busy coroner's pathologist
unless the issues involved are important. Post-mortem angiography is the other
alternative, though where autopsy caseloads are high, this can be difficult to arrange.
Acknowledgements:
www.politie.nl Politiekorpschef @Janny Knol©
www.aived.nl AIVD – @Erik Akerboom ©
www.politie.nl WEB Politie -
@Henk van Essen©
https://www.police-nationale.interieur.gouv.fr/
@ Stephane Folcher ©
Bibliography:
1. Criminal Investigations – Crime Scene
Investigation.2000
2. Forensic Science.2006
3. Techniques of Crime Scene
Investigation.2012
4. Forensics Pathology.2001
5. Pathology.2005
6. Forensic DNA Technology (Lewis
Publishers,New York, 1991).
7. The Examination and Typing of Bloodstains
in the Crime Laboratory (U.S. Department of Justice, Washington, D.C., 1971).
8. „A Short History of the Polymerase Chain
Reaction". PCR Protocols. Methods in Molecular Biology.
9. Molecular Cloning: A Laboratory Manual (3rd
ed.). Cold Spring Harbor,N.Y.: Cold Spring Harbor Laboratory Press.2001
10. "Antibodies as Thermolabile Switches:
High Temperature Triggering for the Polymerase Chain Reaction".
Bio/Technology.1994
11. Forensic Science Handbook, vol. III
(Regents/Prentice Hall, Englewood Cliffs, NJ, 1993).
12. "Thermostable DNA Polymerases for a
Wide Spectrum of Applications: Comparison of a Robust Hybrid TopoTaq to other
enzymes". In Kieleczawa J. DNA Sequencing II: Optimizing Preparation and
Cleanup. Jones and Bartlett. 2006
13. Nielsen B, et al., Acute and adaptive
responses in humans to exercise in a warm, humid environment, Eur J Physiol
1997
14. Molnar GW, Survival of hypothermia by men
immersed in the ocean. JAMA 1946
15. Paton BC, Accidental hypothermia. Pharmacol
Ther 1983
16. Simpson K, Exposure to cold-starvation and
neglect, in Simpson K (Ed): Modem Trends in Forensic Medicine. St Louis, MO,
Mosby Co, 1953.
17. Fitzgerald FT, Hypoglycemia and accidental
hypothermia in an alcoholic population. West J Med 1980
18. Stoner HB et al., Metabolic aspects of
hypothermia in the elderly. Clin Sci 1980
19. MacGregor DC et al., The effects of ether,
ethanol, propanol and butanol on tolerance to deep hypothermia. Dis Chest 1966
20. Cooper KE, Hunter AR, and Keatinge WR,
Accidental hypothermia. Int Anesthesia Clin 1964
21. Keatinge WR. The effects of subcutaneous fat
and of previous exposure to cold on the body temperature, peripheral blood flow
and metabolic rate of men in cold water. J Physiol 1960
22. Sloan REG and Keatinge WR, Cooling rates of
young people swimming in cold water. J Appl Physiol 1973
23. Keatinge WR, Role of cold and immersion
accidents. In Adam JM (Ed) Hypothermia – Ashore and Afloat. 1981, Chapter 4,
Aberdeen Univ. Press, GB.
24. Keatinge WR and Evans M, The respiratory and
cardiovascular responses to immersion in cold and warm water. QJ Exp Physiol
1961
25. Keatinge WR and Nadel JA, Immediate
respiratory response to sudden cooling of the skin. J Appl Physiol 1965
26. Golden F. St C. and Hurvey GR, The “After
Drop” and death after rescue from immersion in cold water. In Adam JM (Ed).
Hypothermia – Ashore and Afloat, Chapter 5, Aberdeen Univ. Press, GB 1981.
27. Burton AC and Bazett HC, Study of average
temperature of tissue, of exchange of heat and vasomotor responses in man by
means of bath coloremeter. Am J Physiol 1936
28. Adam JM, Cold Weather: Its characteristics,
dangers and assessment, In Adam JM (Ed).Hypothermia – Ashore and Afloat,
Aberdeen Univ. Press, GB1981.
29. Modell JH and Davis JH, Electrolyte changes
in human drowning victims.Anesthesiology 1969
30. Bolte RG, et al., The use of extracorporeal
rewarming in a child submerged for 66 minutes. JAMA 1988
31. Ornato JP, The resuscitation of
near-drowning victims. JAMA 1986
32. Conn AW and Barker CA: Fresh water drowning
and near-drowning — An update.1984;
33. Reh H, On the early postmortem course of
“washerwoman’s skin at the fingertips.” Z Rechtsmed 1984;
34. Gonzales TA, Vance M, Helpern M, Legal
Medicine and Toxicology. New York, Appleton-Century Co, 1937.
35. Peabody AJ, Diatoms and drowning – A review,
Med Sci Law 1980
36. Foged N, Diatoms and drowning — Once
more.Forens Sci Int 1983
37. "Microscale chaotic advection enables
robust convective DNA replication.". Analytical Chemistry. 2013
38. Sourcebook in Forensic Serology, Immunology,
and Biochemistry (U.S. Department of Justice, National Institute of Justice,
Washington, D.C.,1983).
39. C. A. Villee et al., Biology (Saunders
College Publishing, Philadelphia, 2nd ed.,1989).
40. Molecular Biology of the Gene
(Benjamin/Cummings Publishing Company, Menlo Park, CA, 4th ed., 1987).
41. Molecular Evolutionary Genetics (Plenum
Press, New York,1985).
42. Human Physiology. An Integrate. 2016
43. Dumas JL and Walker N, Bilateral scapular
fractures secondary to electrical shock. Arch. Orthopaed & Trauma Surg,
1992; 111(5)
44. Stueland DT, et al., Bilateral humeral
fractures from electrically induced muscular spasm. J. of Emerg. Med. 1989
45. Shaheen MA and Sabet NA, Bilateral
simultaneous fracture of the femoral neck following electrical shock. Injury.
1984
46. Rajam KH, et al., Fracture of vertebral
bodies caused by accidental electric shock. J. Indian Med Assoc. 1976
47. Wright RK, Broisz HG, and Shuman M, The
investigation of electrical injuries and deaths. Presented at the meeting of
the American Academy of Forensic Science, Reno, NV, February 2000.







Komentarze
Prześlij komentarz